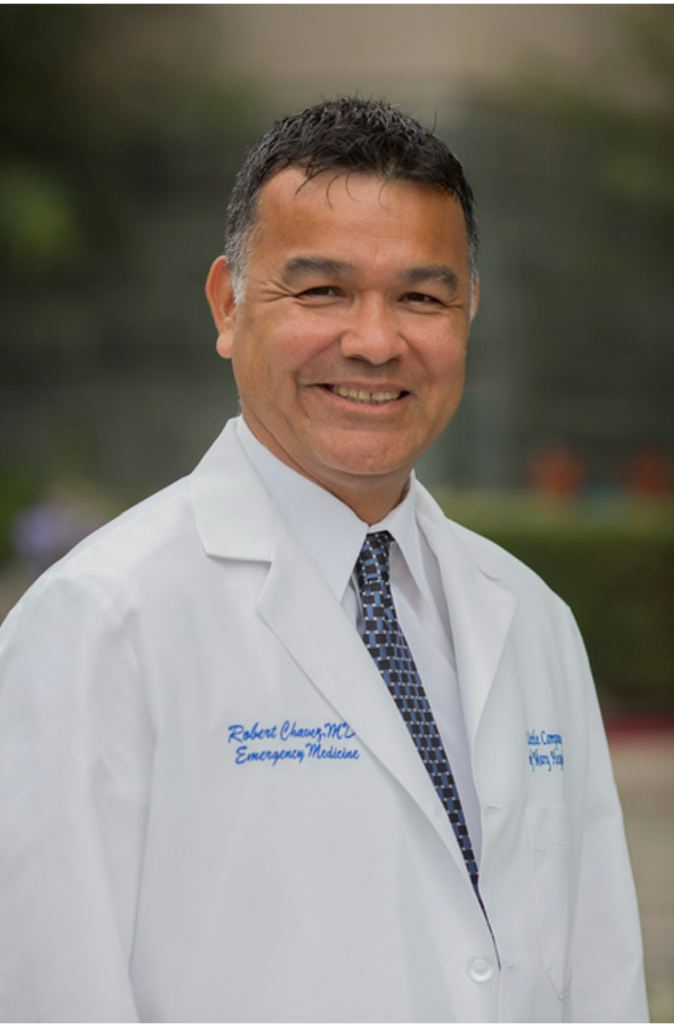
Roneet Lev, MD, FACEP
Executive Director, IEPC
It’s not easy to hang up the stethoscope. For over 30 years, emergency medicine has been a core part of my identity, woven into more than 100,000 patient encounters. It’s never just been a job — I carry it with me everywhere. At home, as a mother and wife, I instinctively triage which child to help first, rule out worst-case diagnoses when someone is ill or injured, and manage the crisis of the day. Prevention is everything: better to treat respiratory distress early than intubate later; better to prevent a child from becoming hangry — or hurt — before it escalates.
Even at 30,000 feet, the call for help draws me in. When someone asks, “Is there a doctor on board?” I’m out of my seat. As my kids grew up, they started volunteering me. Once, my husband and I were seated in first class while our four children were in coach. When a passenger became sick, they immediately volunteered me. My son earned a seat in first class for the rest of the flight, and I spent the duration attending to the patient.
On October 7, 2023, I was at the ACEP Conference in Philadelphia. But I couldn’t focus on any lecture or event. My heart was in Israel, reeling from the most violent and heinous attack on its people since the Holocaust. I did everything I could to get there as an emergency physician. I was fortunate to go several times — training others, supporting a search and rescue team, riding ambulances, and working in emergency departments.
I love emergency medicine. Yes, I’ve been assaulted — twice — knocked to the ground by patients. The SWAT team was called: “911, doctor down.” Yes, I’ve had frustrations with hospital management. I’ve had patients threated to sue me or have me fired. Still, I have no regrets. That’s the nature of the emergency department — it’s intense, unpredictable, and profoundly meaningful. I recommend the specialty to anyone who can multitask, who wants to make an impact with every shift, and who values practical, everyday medical skills. We are medical detectives who overcome any unpredictable challenge thrown our way. Emergency physicians are society’s heroes. The public recognized that during the COVID-19 pandemic — but it’s true every single day, with every patient we care for.
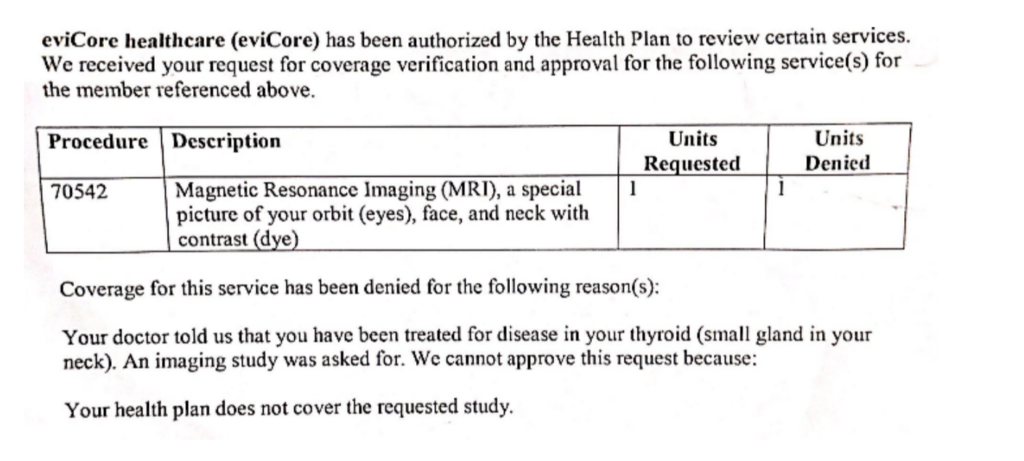
This isn’t how I envisioned ending my EM career. I imagined myself as a little old lady, 5’1” (maybe shrinking to 5’0”), ordering a B52 cocktail at the bedside of a violent, combative patient kicking and spitting — surrounded by six large staff trying to hold them down. But life had other plans. First came thyroid cancer, then a meningioma. I underwent two major surgeries in one year. I’,m proud to say that physically, you wouldn’t know it — but I had to face reality. Could I keep up with fast-paced 10-hour shifts on my feet? Could I adapt to new systems, new computers? (The new computer really stresses me out).
I explored EM-adjacent carer paths. Then, the answer arrived.
I’m honored and grateful to have accepted a position at the White House, in the Office of National Drug Control Policy, where I will oversee public health policies.
Is it challenging to work under a Trump administration? Honestly, no — it’s an honor. Unlike the emergency department, I can eat lunch, take a bathroom break, and am surrounded by excellent security.
This new role requires me to step back from consulting and volunteer work, including my role as Executive Director of IEPC, where I was a founding member. My heart will always be with IEPC, and I’m thrilled to pass the baton to Kavitha Weaver. Kavitha has been part of IEPC since the beginning. She understands the mission deeply and has my full confidence. I know she’ll lead and grow the organization with vision and strength.
Writing this is not easy. It forces me to admit that I am officially hanging up the stethoscope. But one thing I know for sure:
you can hang up the stethoscope — but you never stop being an emergency physician.