James Augustine, MD | Director
Vice President | Emergency Medicine Benchmarking Alliance
Welcome to The Emergency Department Benchmarking Alliance!
The Emergency Department Benchmarking Alliance (EDBA) was created in 1994 for those ED leaders interested in the application of management and service best practices. The Alliance was founded at that time to investigate issues of growing patient volumes and high acuity patients, with unscheduled health needs that were not served in other settings. It has grown into a group of Emergency Department leaders that are dedicated to a high-quality mission; whether their background is pysician, nursing, or administrative. The EDBA is now composed of about 1,500 EDs that saw 45 million patients in 2023.
The vision statement of the EDBA is simple: the Identification, development, and implementation of future best practices in Emergency Medicine.
Attributes of Alliance Members
The Emergency Department is a site of intense service challenges, unpredictable care loads and expectations, and cost challenges. In the healthcare service industry, ED leaders and providers are obligated to a continuous process of quality improvement and patient safety. To mantain this level of service, it is essential to apply the best service concepts in the industry. So EDBA members share materials through an annual survey and active Listserv that promulgates information related to quality medical care, patient satisfaction, staff engagement, medical education, and community service.
The Alliance has ongoing participation by high quality EDs of all volumes and service populations, which collaborate in non-competitive efforts to improve the industry. By fostering community, sharing, support, and mutual advice for people with operational responsibilities in emergency services using a Listserv with 1,400 active members.
Membership in the EDBA is geographic diverse, with members that have recognized expertise in ED operations. The sense of ownership is shared among all disciplines and professionals that provide leadership in an Emergency Department. The attendance of the ED team of physicians, nurses, and administrators cannot be replicated in other groups.
The Alliance makes effective use of the process of “industrial tourism,” and each member has benefited by the firect and non-threatening observation of other ED operations. Alliance members are wired to major events happening throughout the country in emergency practice matters. Ongoing participation of Alliance EDs permits information exchange at a variety of levels, not available through the literature or at offsite meetings. This is an organization that coordinates operations research and health services studies intended to identify best practices.
The EDBA Annual Data Survey
The most critical function of the EDBA is an annual data collection. Since 2004, the Alliance has surveyed its members to collect ED performance data. The data survey represents a broad base of hospital-based EDs, with a separate data report for hospital-affiliated freestanding EDs of EDBA members. The data survey is done rapidly, and includes a full analysis of ED performance for the year, and incorporates the assessment of the latest CDC Emergency Department Survey within the National Hospital Ambulatory Medical Care Survey.
The Alliance has effectively moved the market. The EDBA provides the data to major agencies that are critical to the emergency practice — CMS, the ENA, ACEP, the AHA, The Joint Commission, and a variety of state regulatory bodies. The Alliance has the body of knowledge and data to communicate with general media and other groups that have an interest in ED operations.
The Benchmarking Alliance has conducted annual conferences since 1996 for outside audiences. These conferences feature national speakers on topics relating to Emergency Department “Innovations.” The EDBA conducts the ED Definitions and Performance Measures Summit every 4 years to develop and update the metrics that are needed to manage our industry. This Summit is attended by all major organizations in the industry.
The EDBA seeks regular participation from colleagues engaged in the work of making the ED function at higher levels for patients, medical staffs, hospitals, and communities. This was the most important during the critical early stages of the pandemic.
The Alliance was founded by and remains dedicated to Emergency Department leaders seeking solutions to local service issues. The President of the Alliance is Nick Jouriles, MD. For information on the EDBA, contact Mike Gibbons, the Executive Director, at (855)-622-6674, or visit the website at www.edbenchmarking.org.
The 2023 EDBA Data Report was shared with IEPC members on June 24, 2024.
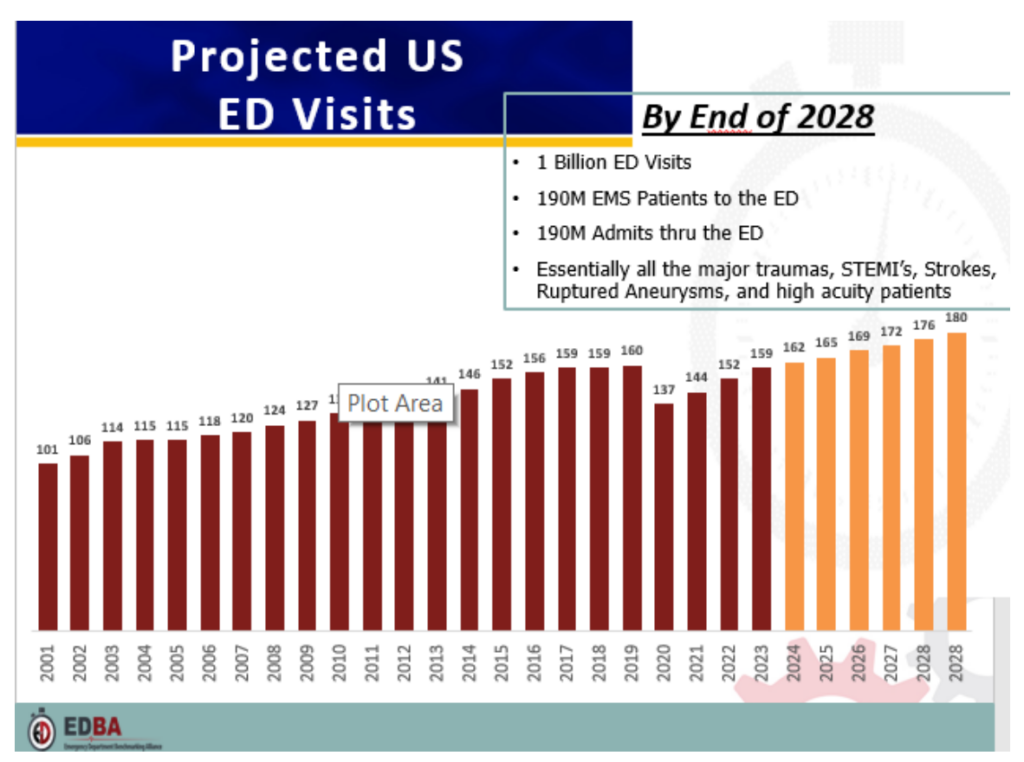
- Volumes collapsed 2020, but ED volume was up from 2022, and across all ED’s is at or above 2019 levels. ED leaders believe the volume increase will continue.
- Outstanding ED work during the pandemic saved hospitals and medical staffs.
- Acuity of ED patients continues to increase.
- The data indicates improved ED flow, although many hospitals still have crippling “Boarding.”
- Mental health cases and ED violence up significantly.
- Walkways may have Decreased.
- Diagnostic testing (especially CT scans) is Increasing.
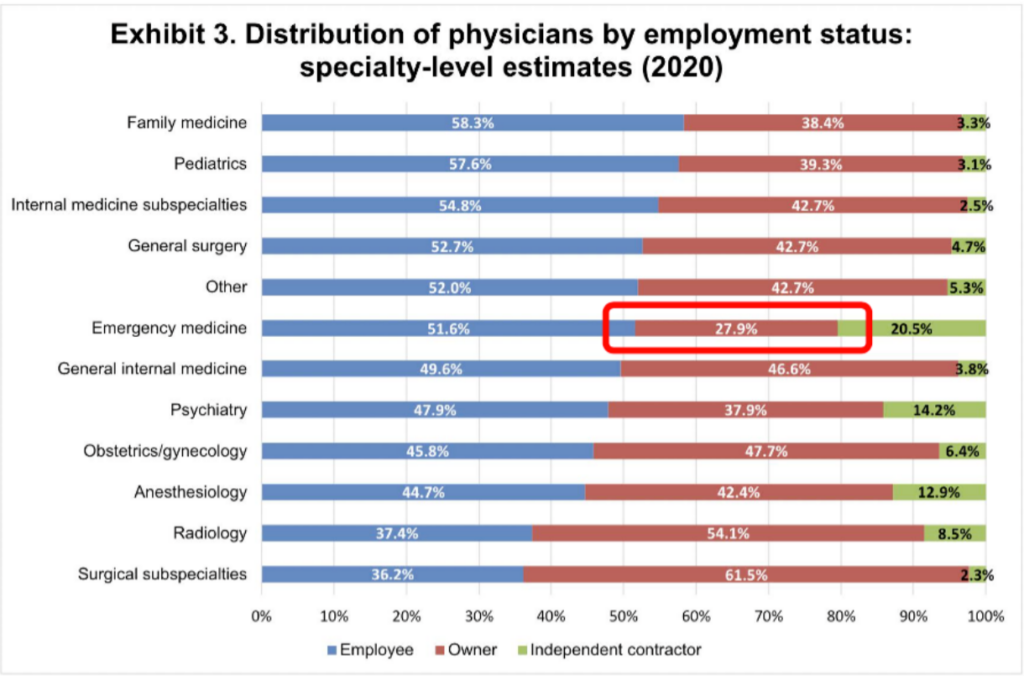
The Volume Expectations are Portrayed in the Graph above.
IEPC Members: IEPC Membership includes EDBA membership. Any IEPC member who wants to access the EDBA website or Listserv conversation, please contact September Liller, Membership Manager, at september@edbenchmarking.com.