Click here to view the PDF of the newsletter.
In This Issue:
- Building a telehealth program in the Emergency Department during COVID-19
- COVID-19 Testing in the Coachella Valley
- Congress Must Pass MAT Act to Save Lives
- Add Fentanyl to your Toxicology Screen
- IEPC Members respond to Legislative Call to Action
- Podcast: ACEP Frontline
- Emergency Care at Risk
Building a telehealth program in the Emergency Department during COVID-19
Casey Grover, MD
Community Hospital of the Monterey Peninsula, Monterey, CA

In March 2020, as COVID-19 rapidly began arriving in the United States, our Emergency Department was working diligently to develop pathways, policies, and procedures to deal with COVID-19. Everyone in our ED was helping to brainstorm; some of our doctors were focusing on airway management, others were focusing on how to avoid exposure at work. However, two of our docs, Dr. Michelle Krueger-Kalinski and Dr. Sameer Bakhda, saw the opportunity to integrate telemedicine into our Emergency Department during COVID-19, and ran with it.
Telemedicine, which is defined as “the remote diagnosis and treatment of patients by means of telecommunications technology”, has an extremely broad set of applications and ways in which it can be used. In our ED, over the last few months, we have created several different ways in which we can use it.
Step 1
We started in the simplest fashion, using telemedicine as “electronic PPE” (aka ePPE) to reduce the exposure of ED staff to patients with COVID-19 and to slow our burn rate of PPE. This was relatively easy to set up. An iPad was placed next to a patient in her/his room, and the ED provider would connect to the patient from her/his smartphone. This would allow for a video chat that allowed the ED provider to see the patient virtually. We started with this for ED providers that were on shift in the ED for patients in the ED – and if there were any issues with the technology, we could easily just put on PPE and go see the patient in person or talk to the person by phone. We started by using the platform Doxy.me – which allowed free, secure, HIPAA compliant video chat.
Step 2
As we gained some experience seeing ED patients while on shift with confirmed or suspected COVID-19 patients via telemedicine, Drs. Krueger-Kalinski and Bakhda took us to the next level with telemedicine: having providers at home see patients in the ED via telemedicine. As we learned about the potential for long quarantines for providers exposed to COVID, we realized we needed to allow docs who couldn’t come in to the ED still help move patients in the ED. Using the same platform, we trialed doctors at home logging into our EHR (EPIC), and signing up for patients with confirmed or suspected COVID. The doctor at home would see the ED patient via telemedicine, ordering tests as needed, and providing the patient with her/his results and discharge instructions via telemedicine. This, obviously, only works with patients who are not seriously ill. Additionally, this has the potential for managing surges in the ED during COVID-19. If we get 15 check-ins in an hour, it would be easy to have a provider at home log in and function as a provider in triage – in a LEAN just-in-time fashion – to get orders started and patients seen via telemedicine.
Step 3
Our ED experienced the nationwide trend in late March and April of record low numbers of patients checking in to our ED. Patients were afraid to come to the ED, and we were seeing very sad cases of people getting really sick by delaying their presentation to medical care. Drs. Krueger-Kalinski and Bakhda took this on as well, developing an ED telehealth follow-up program for our ED. When patients came to the ED and needed subsequent care – such as a wound check for a cat bite to make sure oral antibiotics were working – we developed a pathway to see the patients in follow-up after their ED visit via telemedicine. We worked with our IT team, our Patient Access (registration), and our ED leadership to create this pathway.
Here’s the basic summary:
- ED provider identifies a patient who needs follow-up during an ED visit
- ED provider offers the patient options for follow-up, including ED telemedicine follow-up
- If the patient chooses ED telemedicine follow-up, the ED provider works with ED practice coordinator to set up a follow-up time for the patient
- Patient is registered by Patient Access on the day of the follow-up visit as a “ED TELEHEALTH” patient that shows up in a separate track board on EPIC
- ED provider, from home, logs in and signs up for the patients. She/he does a verbal consent with the patient, ensuring that the patient gives consent for treatment, consent for treatment via telehealth, and consent to bill insurance
- ED provider completes the telehealth follow-up visit, and writes note in EPIC
We’ve been very successful and innovative with these visits. We bought some pulse oximeters to give to patients, and have been seeing COVID+ patients after their ED visit to check their symptoms and pulse ox levels – making sure they are not deteriorating. We even were able to recheck a pediatric abdominal pain – having the parent palpate the abdomen and having the child jump up and down. When we surveyed our patients about their ED Telehealth follow-up visits – almost all of our visits were 5/5 stars – a huge win in getting patients the follow-up care that they need while providing care that patients like and feel has value
Lessons Learned
Having worked through building these various telemedicine pathways for our ED, we’ve found a few major pitfalls. First, not everyone is “technologically gifted”. In Step 1, with patients and providers both on site in the ED, this allowed us to have other people around to help troubleshoot the technology, and the patient could be seen in person as a backup. If I was working and Dr. Smith was having issues with his Doxy.me account, I was happy to help him get it working. When choosing to expand to Step 2 and 3, it’s important that providers and patients both be comfortable using technology to avoid failed telemedicine visits. Second, for providers working from home – it’s important to ensure that patients feel that the encounter is professional. Seeing patients in your pajamas with your child bugging you the whole time is not going to work. Wear professional attire and find a background for your telemedicine encounter that looks clean and professional. Third, keep the telemedicine encounters simple. We initially tried to set up Bluetooth otoscopes and stethoscopes for a nurse to use to examine the patient – and send information to us electronically, only to find that it was a lot of technical work with little change in patient care. Finally, poor video and/or audio quality makes connecting with patients via telemedicine very difficult. Make sure that both the providers and patients have good access to a strong Wi-Fi signal. You can also try some different platforms for telehealth – our providers have used video chat platforms from Doxy.me and Doximity with good success.
COVID-19 Testing In the Coachella Valley
Ian Kramer, IEPC Physician, retired
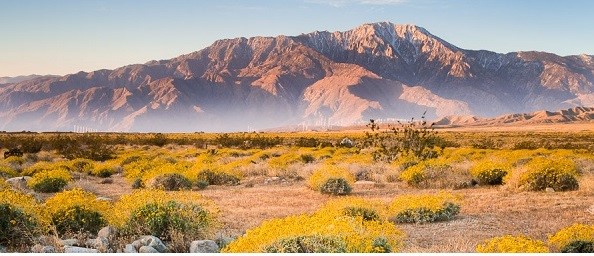
As a volunteer physician in the Coachella Valley, I have participated in a COVID-19 testing program that has been funded by a local Palm Springs artist and spear-headed by our US Congressman, Dr. Raul Ruiz. Dr Ruiz and I are both emergency physicians and work with the Coachella Valley Volunteers in Medicine at our Free Clinic and Street Medicine program.
We tested three separate groups for COVID between late April and May 2020. The initial group was farmworkers in Mecca and a small number of their family members. We had 4 positives out of 125 tests for a rate of 3%. Our second group was our unsheltered homeless population in La Quinta Indio Thermal and Coachella. We tested 50 and had zero positives for a rate of 0%. Our final group was a combination of some farmworkers and mostly residents of Thermal. Out of 175 tests there were 14 positives for a rate of 8%. The farmworkers of Thermal had a much higher positive COVID rate than the unsheltered or farmworkers of Mecca.
It is noteworthy that the temperatures in the Coachella Valley have been in the low 100s and these people work or live outside during the day while the homeless are in tents but not sheltered. The lower incidence of disease may be due to factors such as weather, some moderate social distancing, and our efforts to provide masks sanitizers and education to the community, especially the unsheltered. The Thermal group with a high 8% positive rate included larger families living in confined home likely leading to a higher incidence of disease. We intend to continue testing and monitoring our Coachella residents and will provide a future update.
Congress Must Pass the MAT Act to Save Lives
Roneet Lev, MD President, IEPC

A similar article was recently published in The Hill
Emergency physicians along with the majority of the house of medicine support the Mainstreaming Addiction Treatment Act (MAT), which supports expansion and removing barriers for medications that treat opioid addiction. We need to be able to prescribe medications without bureaucratic restrictions that create barriers for both patients and physicians and that perpetuate the stigma of addiction.
Tragically, the COVID-19 pandemic has increased drug and alcohol use and exacerbated the crisis of addiction in our country. I have intubated more patients with a fentanyl overdose than from coronavirus. If there were a single public health policy that should be endorsed to save the lives of people who struggle with addiction, it would be this act.
The MAT Act will alleviate a serious barrier to treatment of patients who have an opioid use disorder — the Drug Enforcement Administration’s “X waiver.” The waiver prevents physicians from prescribing medications for opioid use disorder (MOUD), such as buprenorphine, without completing an eight-hour course, or a 24-hour course for nurse practitioners and physician assistants. I have treated patients with opioid withdrawal who went to three or four different clinics or emergency departments to find someone who can prescribe MOUD. They were the lucky ones. Many parts of the country have absolutely nowhere to go for treatment. There is no precedence in the medical world for requiring eight or 24 hours of education before prescribing a single medication. Can you imagine creating such a barrier to prescribing insulin or a new treatment for COVID-19?
There are countless physicians who do not find value in a mandated eight-hour course to prescribe a single drug. As someone who has taken the time to take the long course, I don’t blame them — medical providers are spending time keeping up with changing coronavirus treatment recommendations. Furthermore, adding “extra” and a “different” medical standard for treating addiction perpetuates stigma for people who suffer and furthers a false divide between medical health and addiction health.
The historic reasons behind the DEA X waiver regulation stems back to the 1914 Harrison Anti Narcotic Act. This was a time when opium addiction was a problem and the act prohibited doctors and pharmacists from prescribing opioids to people who were addicted to them. In 1974, when soldiers were returning from Vietnam with heroin addiction, Congress acted by allowing DEA to approve a special circumstance to using methadone for maintenance and detoxification of people with opioid use disorder. This opened up opioid treatment programs who used methadone under special DEA licensing and regulation. In 2000, as science and medicine progressed in terms of treating addiction with medication, Congress voted again to keep up with the time by passing the Drug Addiction Treatment Act, known as DATA 2000. This allowed providers to prescribe MOUD if they took the eight- to 24-hour course. It is time for congress to show compassion once again to people with opioid addiction and eliminate the outdated barriers that prevent physicians from prescribing life saving medications.
There are those who will claim that MOUD can be abused or diverted. They are correct. There are many drugs that are abused or diverted from Vicodin, Percocet to Xanax and Suboxone, to name a few. The DEA must continue their important work in preventing illegal activity, but they no longer need to add the X waiver barrier to enforce drug safety.
An overwhelming majority of the house of medicine is behind the MAT Act, with few exceptions. There is an old saying “follow the money” – when looking at who is opposing the MAT Act. Over 20 organizations, including American Medical Association, the American College of Emergency Physicians, the Society of General Internal Medicine, The National Academy of Medicine Consensus Study Report and 22 state public health departments, have submitted letters of support for the MAT Act across the county.
National experts state that MAT medications save lives, and yet the DEA X waiver remains a major roadblock in prescribing. We need congress to pass the MAT Act.
Add Fentanyl to your Toxicology Screen
Roneet Lev, MD President IEPC

This is a request for all emergency physicians and hospitalists to add fentanyl to your urine drug tests. Fentanyl overdoses are the opioid epidemic this year – more than prescriptions or heroin. Please work with your labs to add a rapid fentanyl screen to your toxicology screen. The lab test is not as useful as a send out and frankly should now be part of your standard rapid drug test panel.
Why Add Fentanyl Urine Drug Screen?
- You can assist in a homicide investigation
33-year-old female presented to the ED in cardiac arrest. She was admitted to the ICU on life support. Her differential diagnosis included of MI, PE, and even drug overdose. Her standard urine drug screen was positive for Cocaine, THC, but negative for opioids. Later the local law enforcement overdose team revealed that the patient may have been a victim of homicide as there was a threat to kill her by slipping fentanyl into her drugs. A fentanyl test was added a few days after admission and was positive. However, she received fentanyl as part of her ICU medications. If only she had the fentanyl test done the first time….
- You can confirm your assumed diagnosis
36-year-old man presented to the ED with altered mental status. He received 4 doses of naloxone in the field and 2 more in the ED. He was passed onto the next shift doctor with instructions of “MTF” – metabolize to freedom. Urine tox screen was negative for opioids. Fentanyl is a synthetic opioid that does not show up on regular opioid screens. Fentanyl drug screen was negative too. Alcohol level was 252. He was just drunk and did not need naloxone, buprenorphine or opioid use disorder referral.
- You can save lives besides the one patient in front of you
If you have a patient with COVID the county will do contact tracing to see who else is affected. If you have a patient with diarrhea that is traced to bad lettuce or onions, there will be contact tracing and alerts. If you treatment a patient who overdosed on fentanyl, especially unintentionally, you should think about who else is getting poisoned or killed? Some counties in California are working with special law enforcement teams that do contact tracing for overdoses. They save lives.
- You will learn and become a better doctor
The mix of fentanyl and methamphetamine is a popular combination for agitated delirium. Patient may not have the classic pinpoint pupils and decreased respirations. Patients may complain their feel “weird” after using methamphetamine. That may be because of the contamination of fentanyl without their knowledge. That knowledge will make them careful and even motivate them to seek treatment for their addiction. You will discover that 50% of cocaine and 25% of methamphetamine is contaminated with fentanyl. This data should lead you to prescribe naloxone for these patients.
IEPC Members Respond to Legislative Call to Action
Cassie Chinn, IEPC Communications Director

IEPC has requested members to join the call to action by an emergency physician on both state and federal legislation. It is important for all emergency physicians to be involved to protect your practice and your patients.
The American College of Emergency Physicians is urging members to contact their congressional representative to halt impending Medicare cuts. that could be a 6% cut to emergency physicians in 2021.
Learn more at ACEP Advocacy
Take action: Send a Letter
California ACEP and the California Medical Association is urging members to contact their congressional member to vote against AB 890. This bill will allow nurse practitioners to practice medicine without supervision. We love our NPs, but we also love our patients and loved ones and not willing to compromise on quality of medicine.
Learn more and take action: Send a Letter
Podcast: ACEP Frontline
COVID-19: A Physician Who Got COVID and Lived to Tell the Story
ACEP Frontline, hosted by Dr. Ryan Stanton, features in-depth conversations on the hottest topics in emergency medicine and critical care.
In this episode, Dr. Daniel Lewis discusses his experience actually having COVID-19.
Emergency Care at Risk
Physicians who are small business owners are at risk for extinction by big business consolidation.
Many emergency physicians are small business owners and not hospital or corporate employees. They live and work in the community and have a vested interest to promote the best emergency care for their family and friends. Hospital consolidations and large health insurance companies have threatened the small business practice for physicians who devote their lives to their patients and community.
Giving money to big corporations to distribute for emergency services means giving leverage and tipping the scale in favor of big business over small business emergency physicians. We at IEPC want to protect small business emergency doctors.
Independent Emergency Physicians Consortium, IEPC is a group of small business emergency department owners who collaborate for best practices for their patients and community. As small business owners we are more cost efficient by eliminating middle management, recruitment fees and large overhead expenses.
